Introduction
Gingival growths are among the most frequently encountered lesions of the oral cavity. One of the infrequently occurring gingival tumour is Peripheral Ossifying Fibroma. It is an uncommon non neoplastic tumour like growth of the gingival tissues that represents up to 9.6% of all gingival tumors and up to 3.1% of all oral lesion that are biopisied.[1] Other terms used to describe this lesion are peripheral fibroma, fibrous epulis, ossified fibrous epulis or peripheral cementifying fibroma etc[2]. They are two types of ossifying fibromas: the central type and the peripheral type. The central type arises from the endosteum or the periodontal ligament adjacent to root apex and causes expansion of the medullary cavity. The peripheral type occurs solely on the soft tissue covering the tooth bearing areas of the jaws. Peripheral Ossifying Fibroma lesions appear as nodular masses either pedunculated or sessile .The colour of the growth ranges from red to pink and the surface is frequently but not always ulcerated. Intraoral ossifying fibromas often occurs in female patients (Female :male ratio =1.22:1) and predominantly in the 2nd or 3rd decade of life. There is high predilection of maxillary anterior region as compared to mandible .
Oral Peripheral ossifying fibroma usually present as focal, reactive, non-neoplastic tumor-like growth of the soft tissue that often arises from the interdental papilla[3]. These are slowly growing painless growths in the gingiva. Trauma or local irritants such as dental plaque, calculus, micro-organisms, masticatory forces, ill-fitting dentures and poor quality restorations have been implicated in the etiology of peripheral ossifying fibroma.[4] There is uncertainity regarding the etiopathogenesis of these lesions and they are initiated due to overproduction of the fibrous tissues in the periodontal connective tissues. It is believed to derive from the multipotential mesenchymal cells of the periodontal ligament which are able to form cementum, bone and fibrous tissue.[5]
Clinical Case Presentation
A 60 year old female patient reported to the Out Patient Department of Periodontology and Implantology DAV ( C ) Dental College and presented with the chief complain of a painless firm swelling in the lower anterior teeth region since 2 years, the lesion started as a very small nodule and had gradually increased to attain the present size (Figure 1 & Figure 2). Patient had problem during mastication, speech as well as aesthetics due to its present giant size. The medical history was unremarkable and a thorough examination revealed incompetent lips and otherwise normal facial features. Introral examination showed that there was an oval, hard, pedunculated growth located on the labial surface of the gingiva in relation to 31-43 region; measuring approximately 2x 1.5 cm in diameter. The overlying mucosa was reddish pink in color, On palpation, the mass was firm in consistency, pedunculated, non-tender and no bruit or pulse was felt. The oral hygiene status of the patient was also very poor.
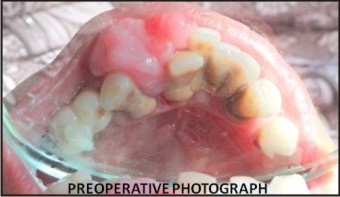 | Figure 1 : Preoperative Photograph
 |
 | Figure 2 : Preoperative Photograph
 |
On periodontal examination underlying teeth had bands of supragingival and subgingival calculus and probing pocket depth of 6mm in relation to 31,32,41,42 and 43 region. All the records were made using digital radiographs & photographs. A diagnosis of Chronic Generalised periodontitis with a tumour like growth in the mandibular anterior region was made.
The patient was made aware of all the possible treatment options for the lesion. The treatment plan included initially scaling and root planing (Phase I therapy) and subsequently excision of the lesion was planned. Surgery was performed only following re-evaluation of the Phase I therapy. A written informed consent was saught and under local anaesthesia, an extensive excisional biopsy was performed and the underlying surface was thoroughly curetted up to the bone. After controlling the bleeding, the surgical site was sutured and covered using Coe-pack. Post-operative instructions were given and the patient was recalled for post operative re-evaluation after 1 week. The one week follow up was uneventful with the surgical site showing signs of healing. The entire tumour mass excised (Figure 3) was subjected to histopathology examination which confirmed the diagnosis of oral peripheral ossifying fibroma. A six month postsurgical follow-up of the patient showed no evidence of recurrence (Figure 4).
 | Figure 3 : Excised Tumour Mass
 |
 | Figure 4 : Post Operative Photograph
 |
Discussion
Intraoral ossifying fibromas have been described in the literature since 1940’s . Many names have been given to similar lesions, such as epulis, peripheral fibroma with calcification, peripheral ossifying fibroma, calcifying fibroblastic granuloma, peripheral cementifying fibroma, peripheral fibroma with cementogenesis and peripheral cemento-ossifying fibroma.[6]
Gardner in 1982 coined the term peripheral ossifying fibroma for a lesion that is reactive in nature and is not the extraosseous counterpart of central ossifying fibroma[7]. Peripheral Ossifying Fibroma is a non-neoplastic enlargement of the gingiva with randomly distributed calcifications, immature bone and osteoid. It is found exclusively on the gingiva and does not arise in other oral mucosal location. Ossifying Fibroma is a slow growing well circumscribed painless mass usually presenting itself in the 2nd or 3rd decade of life. Clinically, it resembles a peripheral fibroma, but histopathologic analysis always reveals immature bone and osteoid within the lesion.
Peripheral Ossifying Fibroma is an uncommon lesion of the gingival tissues that chiefly arises from the interdental papilla and represents upto 9.6% of all gingival tumors. It accounts for up to 3.1% of all oral lesion that are biopisied . It varies from pale pink to cherry red in color, can be either pedunculated or sessile and is typically located in the interdental papilla region and surface may occasionally show ulceration[8]. The tumour may cause a separation of the adjacent teeth, and occasionally minimal bone resorption can be seen beneath the lesion. The peak incidence is found most frequently in teenagers and young adult females(Female:Male=1.22:1) and some studies have reported that women are 2-4 times more likely to be affected than men.[3] These lesions have high predilection for occurrence in maxillary anterior region compared to mandible.[9]
The etiopathogenesis of Ossifying Fibroma is unclear, trauma or local irritants such as subgingival plaque and calculus, dental appliances, poor-quality dental restorations, microorganism, masticatory forces, food lodgment and iatrogenic factors are known to influence the development of the lesion. Hormonal influences may play a role, given the higher incidence of Peripheral Ossifying Fibroma among females, increasing occurrence in the second decade and declining incidence after the third decade[10]
An origin from cells of periodontal ligament has been suggested because of exclusive occurrence of Ossifying Fibroma from Interdental papilla, the proximity of gingiva to PDL, the presence of oxytalan fibers within the mineralized matrix of some lesions, the age distribution, and the fibro cellular response similar to other reactive gingival lesions of periodontal ligament origin . Early Perpheral Ossifying Fibroma presents as ulcerated nodules with little calcification allowing easy misdiagnosis as a pyogenic granuloma. It should be differentiated from fibrous dysplasia, cemento-osseous dysplasia etc.
In our case the lesion presented in an unusual location, in the mandibular anterior region involving the incisors and it originated from the interdental papilla between 42- 43, in a female patient aged 60 with chronic generalized periodontitis. She presented with poor oral hygiene and exhibited moderate amounts of supra and sub-gingival calculus in the proximity of the lesion. Peripheral Ossifying Fibroma can produce migration of teeth with interdental bone destruction. In our patient the teeth exhibited spacing between 42-43 and the growth appeared to originate from the interdental papilla between 42-43. The large lesions may occasionally cause displacement of the mandibular canal if encountered in the posterior mandibular region.[11]
The differential diagnosis for peripheral ossifying fibroma included pyogenic granuloma, central ossifying fibroma, peripheral odontogenic fibroma, irritational fibroma. On histopathological examination peripheral ossifying fibroma exhibits fibrocellular connective tissue stroma surrounding mineralized mass. This fibrocellular proliferation is accompanied by an inflammatory component of lymphocytes, plasma cells and multinucleated giant cells. Lesion was not encapsulated and revealed bone forming osteoblasts and cementoblasts in the fibrous connective tissue stroma. The calcified mass comprises of woven bone ,cellular cementum or a mixture of woven and lamellar bone. These features support the theory that peripheral ossifying fibroma develops from undifferentiated mesenchymal cells. These cells are derived from periodontal ligament or periosteum of the adjacent teeth and have inherent proliferative potential to form bone or cementum[12]
Treatment of Ossifying Fibroma consists of aggressive surgical excision along with involved periodontal ligament and periosteum along with elimination of etiological factors, scaling of adjacent teeth in an attempt to minimize the possibility of recurrence . Studies have reported high rate of recurrence (8% to 20%) of peripheral ossifying fibroma. Various reasons for the reoccurrence of peripheral ossifying fibroma have been suggested. They include the incomplete removal of the lesion, the failure to eliminate local irritants and difficulty in accessing the lesion during surgical manipulation as a result of the intricate location of the lesion (usually an interdental area). Close postoperative monitoring is required in all cases of Peripheral Ossifying Fibroma that have been treated with surgical excision.
Conclusion
The peculiarity of the presented case is the intriguing since the predilection of peripheral ossifying fibroma is in maxillary anterior region than in mandibular area. Also the occurrence of Ossifying Fibroma in an elderly female patient in her post menopausal phase is in contrast to its common occurrence in a young females. The clinician therefore has to look beyond the usual norms of gender, age and site predilection to arrive at a clinical diagnosis. Further, histologic investigations are integral for its confirmation.
References
1. Canger EM, Celenk P, Kayipmaz S, Alkan A Gunhan O. Familial ossifying fibromas: report of two cases Journal of Oral Science 2004; Vol. 46(1): 61-64.
2. Moon WJ, Choi SY, Chung EC, Kwon KH, Chae SW . Peripheral ossifying fibroma in the oral cavity: CT and MR findings. Dentomaxillofac Radiol 2006;(36):180-182.
3. Farquhar T, Maclellan J, Dyment H, Anderson RD. Peripheral ossifying fibroma: a case report. J Can Dent Assoc 2008;(7):809-12.
4. Miller CS, Henry RG, Damm DD. Proliferative mass found in the gingiva. J Am Dent Assoc 1990;(121):559-60.
5. Kumar SK, Ram S, Jorgensen MG, Shuler CF, Sedghizadeh PP. Multicentric peripheral ossifying fibroma. J Oral Sci 2006;(48):239-43.
6. Feller L, Buskin A, Raubenheimer EJ. Cemento-ossifying fibroma: case report and review of the literature. J Int Acad Periodontol 2004; 6(4):131–5.
7. Gardner DG. The peripheral odontogenic fibroma: an attempt at clarification. Oral Surg Oral Med Oral Pathol 1982;54(1):40-8.
8. Neiville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 2nd ed. Philadelphia;W.B. Saunders,2004;451-52.
9. Kenney JN, Kaugars GE, Abbey LM. Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibroma. J Oral Maxillofac Surg 1989; 47(4):378–82.
10. Yadav A, Mishra MB. Peripheral Cemento-ossifying Fibroma of mandible: A case report Indian J Stomatol 2011;2(3):193-196.
11. Bertolini F, Caradonna L, Bianchi B, Sesenna E. Multiple ossifying fibroma of the jaws: a case report. J Oral Maxillofac Surg 2002;60:225-229.
12. Marcos JA, Marcos MJ, Rodriguez SA, Rodrigo JC, Poblet E Peripheral ossifying fibroma: A clinical and immunohistochemical study of four cases. Journal of Oral Science 2010;52(1):95-99.
|